Cartilage is a smooth, firm tissue that reduces friction between bones and other tissues. It’s found in joints between bones, such as the knee joint, where it acts as a shock absorber.
Cartilage wears out over time. When cartilage wears away, it causes pain and inflammation in the joints. This is called chondromalacia (pronounced: kon-droh-ma-lay-shah). Chondromalacia causes the underlying bone to rub against the bone underneath it, causing pain and swelling.
Cartilage damage can also lead to osteoarthritis (also called degenerative joint disease). Osteoarthritis affects up to half of all Americans over age 60. When you have osteoarthritis, your cartilage breaks down and becomes less effective at cushioning bones from one another as they move around inside your joints. As this happens, more stress is placed on your bones themselves, which can cause them to wear down faster than normal because they don’t have enough cushioning support from the cartilage.
Cartilage Wear On Knee
Both the femur (thigh bone) and tibia (shinbone) are covered with small, white, well-lubricated articular cartilage that makes the knee joint glide and function well. Healthy articular cartilage is a central component of a normal healthy joint.
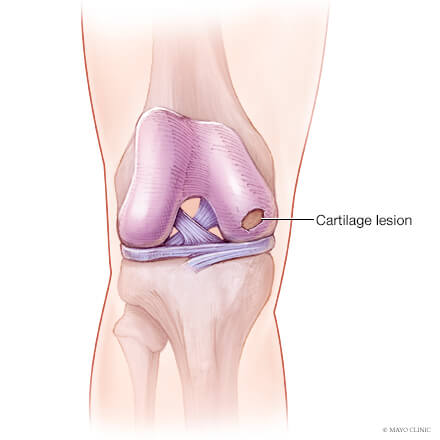
Cartilage can become damaged due to a trauma such as a pivoting sport or when turning the knee or bending it deeply. Cartilage can also come loose due to damage in the underlying bone, OCD, or osteonecrosis. Sometimes cartilage damage occurs as part of degeneration, called osteoarthritis, which is the overall loss of tissue quality that occurs with aging.
Cartilage damage is most frequently seen between the ages of 15 and 30 or above the age of 50.
Damaged cartilage can lead to short-term symptoms such as pain, swelling, locking symptoms, and longer-term symptoms of osteoarthritis due to lack of the shock absorber function.
Knee cartilage damage

A common type of injury that can be caused suddenly from a sports injury or come on gradually with conditions such as arthritis.
The bones of your knee joint are coated with a layer of slippery tissue called cartilage, which reduces friction as the bones move over each other. Cartilage can be damaged or torn as a result of an accident or conditions such as arthritis.
Knee cartilage damage can be caused by a sudden twisting movement or a direct impact to the knee – both of which happen in sports such as rugby, squash, football or skiing.
Arthritis is a common cause of knee cartilage damage. There are two main types of arthritis:
- osteoarthritis – a degenerative condition that wears away bone and cartilage.
- rheumatoid arthritis – an inflammatory disease causing swelling and stiffness in your joints, which can damage the bones and cartilage.
Minor cartilage damage can get better on its own after a few days, although more serious injuries or conditions will need treatment.
Cartilage has very little blood supply, meaning it is hard for it to repair itself. Surgery is usually the only option for more serious damage.
Symptoms of knee cartilage damage

The symptoms of knee cartilage damage are similar to other common knee injuries:
- joint pain – this may continue even when resting and worsen when you put weight on the joint. J oint pain – this may continue even when resting and worsen when you put weight on the joint
- swelling – this may not develop for a few hours or days
- stiffness
- a clicking or grinding sensation
- the joint locking, catching, or giving way
Diagnosis of knee cartilage damage
Many knee conditions that have similar symptoms, and the damage can be done in very similar ways (sudden twisting or wrenching, blow to the knee, arthritis).
Because of this, your doctor will carefully examine your knee and will often recommend an MRI scan and/or weight bearing X-rays to determine the cause of the problem.
Treatment of knee cartilage damage
Non-surgical options
To manage pain and swelling in the days immediately after an injury:
- take over-the-counter anti-inflammatories (eg ibuprofen)
- ice your knee two to three times a day, for 20 mins at a time
- elevate your leg as much as possible
- support your knee as it recovers by wearing a knee brace
One of our physiotherapists can also give you exercises to help regain motion and build up muscle strength around the knee.
Surgical options
If your cartilage damage is severe or not responding to physiotherapy, your orthopaedic surgeon might recommend surgery.
Keyhole surgery – Your surgeon repairs damaged cartilage by inserting surgical instruments through small cuts in your knee. The operation is carried out using a tiny video camera inserted into your knee and a monitor. Cartilage repair can involve shaving or cutting off ragged edges of torn tissue. If the cartilage doesn’t need replacing, your surgeon may drill small holes in the surface of the bone to encourage the cartilage to re-grow in place. In some cases, cartilage from another part of your body can be grafted onto the bones.
When You Have No Cartilage in Your Knee
Cartilage in the knee begins to wear down over time from repetitive stress to the knee joint. Prolonged sitting and standing often result in increased discomfort, and weight-bearing activities like walking, squatting, and going up and down stairs can be very challenging and painful without adequate cartilage for cushioning and support.1
The most common cause of loss of cartilage in the knee joint is knee osteoarthritis. When cartilage loss is severe, standing and walking can become very difficult due to pain. Cartilage loss in the knee joint can also result from injury to the knee, including anterior cruciate ligament (ACL) ruptures, meniscus tears, and patellar (kneecap) dislocations that increase the risk of cartilage damage and development of knee osteoarthritis in the future.1
What Is the Function of Cartilage?
Cartilage is a form of connective tissue that covers the end of each bone in the body. It provides cushioning and shock absorption to the joints, allowing them to move smoothly without restriction. When there is decreased cartilage within a joint, you may experience pain, stiffness, and difficulty moving your joints through their full range of motion.
A variety of treatments are used to treat loss of cartilage in the knee, ranging from conservative measures like pain medications, weight loss, and physical therapy to more invasive procedures like injections and surgery, depending on the severity of your symptoms and degree of cartilage loss.
:max_bytes(150000):strip_icc():format(webp)/GettyImages-1180607422-b02972c6761641e1a4315f1739b0fa54.jpg)
Weight Loss
Increased body weight places an increased amount of pressure on the knee joint with weight-bearing activities like standing, squatting, walking, and going up and down stairs. Each extra pound of weight can put up to six additional pounds of pressure on the knees with physical activity. People who are overweight also tend to develop osteoarthritis at an earlier age with greater severity of symptoms compared to those at a healthy weight.1
An increased amount of fat cells within the body also stimulates an elevated insulin response and inflammatory processes throughout the body that increase the rate of cartilage cell degradation. Losing extra body weight can help decrease symptoms of cartilage loss by reducing the pressure applied on the knee joints and slowing down inflammatory processes caused by metabolically disrupting fat cells.2
Braces
If cartilage loss is localized to one side of the knee—most commonly the inside of the knee joint—specialized, custom-made braces can help reduce pressure on the knee joint and improve alignment of the knee.
An unloader knee brace stabilizes the knee to limit side-to-side movement while allowing the knee to bend and extend without limitation. The brace also contains three pressure points that push the knee away from the area of cartilage loss to decrease compression at the joint surface. Knee braces are strongly recommended for the treatment of knee osteoarthritis to help decrease pain and improve function.3
Medication
NSAIDs
Over-the-counter pain relieving medications such as acetaminophen (Tylenol) and ibuprofen (Advil) or anti-inflammatory medications like naproxen sodium (Aleve) can help reduce pain, swelling, and inflammation in the knee joint.3
If symptoms are severe enough, your healthcare provider may prescribe a higher dosage of a nonsteroidal anti-inflammatory drug (NSAID) to help decrease your knee pain so you can sit, stand, and walk with less discomfort.
Corticosteroid Injections
Corticosteroids, or cortisone injections, are anti-inflammatory medications that can be injected into the knee joint to reduce pain, swelling, and inflammation. They are the most commonly used type of knee injections for treating knee pain from osteoarthritis.3
Corticosteroid injections are performed under local anesthesia, where you will be awake for the procedure but your knee will be numbed. A small amount of anesthesia will be injected into your knee before the corticosteroid, which usually begins to work two to three days later.3
Corticosteroid injections can help relieve pain and reduce symptoms between six weeks and six months, although the injections are not effective for everyone. You will typically not be allowed to receive more than two or three injections per year.
Corticosteroid injections may not be recommended for patients who have diabetes or other problems with blood sugar since corticosteroid use can raise blood sugar levels.
Viscosupplementation
Viscosupplementation, sometimes called gel injections, refers to the use of injecting hyaluronic acid into the knee to decrease pain and improve joint movement. Hyaluronic acid used for injections is derived from the combs of chickens.4
Hyaluronic acid is a gel-like substance that occurs naturally in the synovial fluid within each joint capsule that surrounds all joints. It serves as a lubricant that allows bones to move smoothly within a joint and provides shock absorption to decrease pressure and friction within joints. Over time, hyaluronic acid levels in the joints decrease, especially as the joints wear down with osteoarthritis.
With viscosupplementation, you may receive between one and five injections. If there is excess swelling and fluid buildup in the knee joint, your healthcare provider will use a needle to aspirate, or remove, the fluid before injecting the hyaluronic acid. You should avoid prolonged standing, walking, jogging, running, or heavy lifting for the first 48 hours after receiving a hyaluronic acid injection.4
For patients who report pain relief following hyaluronic acid injections, it may take up to four weeks to notice any significant improvement, and the lasting effects can vary from two to six months. Hyaluronic acid injections may be repeated about every six months.4
Hyaluronic acid may be recommended for patients with diabetes who have knee osteoarthritis because hyaluronic acid injections do not raise blood sugar the way corticosteroids do.
Physical Therapy
Physical therapy plays an important role in decreasing symptoms and preventing the progression of cartilage loss in the knees. A physical therapist will evaluate your knee and hip alignment, muscle strength, range of motion, and movement patterns to develop an individualized plan of care to address your limitations.
The muscles surrounding the knee help support the knee joint. When they are weak, the bones of the knee joint are subject to increased pressure and a higher risk of cartilage breakdown. Strengthening the muscles around the knees and hips helps offload the knee joint and support your body weight so that less pressure is applied to the joint surfaces and surrounding cartilage.3
Surgery
Knee arthroscopy is the most common type of surgical procedure performed to repair, remove, or replace damaged cartilage in the knee joint that can be causing pain and limiting range of motion of the knee joint.
During knee arthroscopy, a surgeon uses an arthroscope—a tool about the width of a pencil with a camera and light attached—to view the inside of your knee joint. This allows the surgeon to examine the inside of the knee joint without making a large incision along the outside of the knee, which is performed with open knee surgery.5
Knee arthroscopy helps protect the knee joint from the risk of infection by decreasing exposure of the joint to the outside environment, and often results in an improved cosmetic appearance of the knee by reducing the size of the surgical incisions and resulting scar formation. Knee arthroscopy also protects the surrounding knee structures, including skin, muscle, tendons, and ligaments from being damaged due to the smaller incisions.5
Different types of arthroscopic knee procedures to manage loss of cartilage include microfracture surgery, autologous chondrocyte implantation, and osteochondral autograft transplantation.
Microfacture
With microfracture surgery, a surgeon will use a drill to create mini fractures in the bones of the knee joint after removing an area of damaged cartilage. Creating small holes in the bone helps stimulate bone marrow cells, which can help spur the growth of new cartilage cells.
Microfracture surgery has variable outcomes since the new cartilage that forms is often fibrocartilage rather than hyaline cartilage, the type of cartilage that covers joint surfaces. Fibrocartilage is denser and not able to withstand the same force demands as hyaline cartilage. As a result, it provides less cushioning and pressure relief and has a higher risk of breaking down after one or two years.
Autologous Chondrocyte Implantation
Autologous chondrocyte implantation involves removing cartilage cells arthroscopically and then growing them in culture in a laboratory for four to six weeks. These new cells are then reimplanted into the knee in areas of damage during another surgery to promote new growth of cartilage.
Osteochondral Autograft Transplantation
Osteochondral autograft transplantation involves removing intact cartilage cells from healthy areas of the knee joint and transplanting them to areas of damage. This procedure is typically only used in areas of focal damage localized to a specific area that is 10 to 20 milimeters in size. Because osteochondral autograft transplantation is not used to treat widespread cartilage damage in the knee joint that is characteristic of osteoarthritis, most candidates for this type of procedure are younger than 50 years old who have cartilage damage as a result of direct knee joint trauma.
Total Knee Replacement
Approximately 54% of all Americans diagnosed with knee osteoarthritis will undergo total knee replacement to treat their symptoms. A total knee replacement is often the last resort used to treat severe symptoms of knee osteoarthritis when the cartilage of the knee joint has significantly worn down, limiting everyday activities and making standing, walking, and going up and down stairs very challenging and painful.1
During the operation, a surgeon will make a long incision down the center of the knee to access the knee joint. The kneecap will be moved aside to expose the ends of the femur, the upper leg bone, and tibia, the lower leg bone. The ends of each bone will be shaved off and capped with metal hardware that is screwed into the leg bones. These metal components replace the damaged joint surfaces of the knee that have degenerated over time due to cartilage loss.1
Nutritional Supplements
Certain dietary supplements can help support healthy cartilage cells to protect the knee joint from wear and tear. Glucosamine and chondroitin can help repair damaged cartilage in the hip joint and prevent enzymes from further breaking down cartilage. Vitamin D3 is also important for maintaining good bone health and supporting immune system functioning to decrease inflammation throughout the body.3
Complications
Loss of cartilage within the knee joint can result in complications affecting the integrity of the knee joint surface due to increased pressure demands, which can lead to the development of bone spurs, subchondral bone sclerosis, and cysts and lesions.
Bone Spurs
Bone spurs, called osteophytes, are outgrowths of bone that develop within joints due to increased pressure between bones from lack of cartilage. Bone spurs are common in the knee since it is a major weight-bearing joint that withstands high pressure demands.6
Without adequate cartilage, the bones of the knee become irritated and inflamed due to increased pressure and friction with movement and weight-bearing of the leg. Bone cells react to this increased pressure by producing more bone growth in an attempt to provide more protection to the joint, forming bone spurs that can change the appearance of the joint and limit mobility by restricting movement.6
Subchondral Bone Sclerosis
Subchondral bone is the type of bone directly under the cartilage at the ends of bones. Sclerosis is the process of abnormal hardening or stiffening of body tissues that can occur in multiple structures, such as arteries, nerves, and bones. Subchondral bone sclerosis in the knee occurs when the bones at the end of the femur and tibia that join to form the knee joint thicken as a result of becoming exposed from loss of cartilage.6
Similar to how bone spurs form, subchondral bone cells react to increased pressure within the knee joint from cartilage loss by producing more bone growth in an attempt to provide more protection to the joint. The damaged bone grows back thicker than before as the body tries to repair the damage, similar to thickened scar tissue that develops after an injury. Bone spurs are also common with subchondral bone sclerosis in addition to the subchondral bone thickening.6
Cysts and Lesions
As a result of damage to subchondral bone from cartilage loss, further damage can occur to the remaining cartilage from lack of cushioning in the knee, causing lesions or tears in the remaining cartilage. Subchondral cysts—abnormal growths of fluid-filled sacs—can also develop in the subchondral bone, which may be painful and limit proper mobility of the knee joint.
Coping
Ongoing knee pain and disability from cartilage loss can be frustrating, but there are ways you can cope with an injury or conditions like osteoarthritis. Maintaining healthy lifestyle habits to reduce inflammation and stress to the joints can help make it easier to manage symptoms and prevent worsening of cartilage loss.
Ways to cope with cartilage loss include:3
- Getting at least seven to eight hours of uninterrupted sleep at night
- Eating a healthy diet of whole, natural foods
- Managing a healthy weight and lean body mass through diet and exercise
- Staying adequately hydrated
- Maintaining a positive attitude and managing stress in healthy ways
- Staying connected to others for social support
- Resting your knee joints to decrease pain and inflammation
- Limiting high impact and repetitive activities that stress the knee joint, such as running and jumping
Loss of cartilage in the knee can cause irreversible damage to the underlying bones that form the knee joint. If you have experienced injury to the knee or are in the beginning stages of developing osteoarthritis, it is important to seek medical attention to receive guidance and treatment for managing the effects of cartilage loss and preventing progression to further damage.
Osteoarthritis is a degenerative condition that tends to get worse over time, but by taking care of your body and strengthening the muscles that support your knee, you can help prevent further damage to your knee joint and cartilage to stay active and pain-free.



